When developing a medical device or pharmaceutical, we often jump to thoughts of getting approval from a regulatory authority (e.g., FDA or CE). However, in order to get that approval and be able to sell your product, everything leading up to the request for approval has to be objectively defined complying with the most strict reliability standards. This is where Good Laboratory Practice Comes in. Without GLP-compliance, receiving approval based on your pre-clinical trials, will be very hard to achieve.
If this sounds intimidating, it should. That is why we are writing this discussion and that is also why it is ultimately important to work with a CRO that has the experience, knowledgebase and expertise to take your product on its journey.
Good Laboratory Practice (GLP), is a quality system of management controls for research laboratories and organizations to ensure the uniformity, consistency, reliability, reproducibility, equality and integrity of products in development for human or animal health through non-clinical safety tests. From physio-chemical properties through acute to chronic toxicity tests.1
When we think of regulations and standards, our first thoughts are often of the FDA or the CE. However, the concept of GLP was first introduced in New Zealand and Denmark in 1972, and then by the US in 1978 and the OECD in 1992.
The US introduced GLP in direct response to a scandal, known as the Industrial BioTest Labs scandal. Ironically, IBT Labs were a product safety testing lab. They did most of the testing for pharma, chemical and industrial companies through the 1950’s, 60’ and 70’s, performing about one third of toxicology testing in the US. In the early 1980’s they were found to be engaging in scientific fraud. Incidentally, this also led to the regulation of pesticides in North America.
GLP is a set of standards created to prevent such fraud by applying accepted methods for conducting all activities and operations in the lab to ensure proper safety and quality of the product. It follows then, that GLP is also part of the bigger concept of quality assurance and control. GLP is a system of quality management controls for non-human research laboratories. The goal of GLP, is to guarantee that non-clinical safety tests are of quality, consistency, reliability and uniformity. 2
GLP also provides an outline for showing how pre-clinical studies should be performed, evaluated and reported, thus supporting the validity of the resultant data.
What fields/what products need to follow GLP?
There are several industries that must follow GLP, such as pharmaceuticals, biologics, medical devices, food additives, pesticides and chemicals.
GLP specifically applies for: non-clinical lab studies used to support research applications or FDA marketing permits; EPA regulated pesticides; Toxic Substance Control Act-regulated chemicals.
For our purposes, we will focus on pharmaceuticals, biologics and medical devices.
Components of GLP
As you can imagine, GLP has many components. Each of them has its own requirement. Most references for GLP will include at least 9 components (10 are assembled here)3
- Personnel – All personnel working in the course of the study must have fulfilled and maintain training requirements. All of their qualifications, including job description and GLP training must be documented and maintained. All personnel must also be familiar with, and follow Standard Operating Procedures (SOPs).
- Test Facility Management – For each GLP study, the facility where the study is being conducted must have a designated study director and an independent Quality Assurance Unit (QAU).
- Study Director – The Study Director is the individual, appointed by the Test Facility, who is responsible for leading the study, The Study Director is responsible, for ensuring that the study complies with all GLP requirements.
- QAU – The Quality Assurance Unit must inspect the study throughout, maintaining written records of inspections and providing status reports to the Test Facility’s management and to the Study Director.
- Facilities – Test Facilities have to be suitable in size, construction and design, as well as providing enough separation between subjects.
- Equipment, including software – All equipment must be appropriately designed, sized, maintained, regularly tuned and adjusted, and validated according to GLP requirements.
- Test Facility Operation – There must be written, accurate, current, approved and available SOPs for all procedures.
- Protocol – The protocol (study plan) must contain the objectives and methods of the GLP-compliant study. It must be approved by the Study Director, Test Facility’s management representative, QA representative and the sponsor’s representative. The Study Director is responsible for instructing all personnel involved in the study on the protocol, and for making sure it is carried out accordingly.
- Records and Reports – All study materials including raw data, protocols, final reports and specimens must be recorded and kept.
- Storing and Archiving – All records and reports of the GLP study must be stored and archived according to GLP requirements, preserved and ready for retrieval at any time.
Standard Operating Procedures (SOP)
SOPs are of paramount importance and as such, they must be implemented accurately, and exact records of their implementation must be kept. When thinking of SOPs, it is best to think in terms of more, rather than less. The list below is considered minimalistic of what your SOP records should contain.4
- Test and control/reference articles (items) – This includes the receipt, identification, storage, handling, mixing and sampling -essentially, everything related to the test and control/reference articles.
- Observations – written observation of the test system must be applied, recorded and kept.
- Lab tests – all records and listings of all lab tests. While this may seem obvious, it is essential that precise records are kept of all lab tests.
- New method development and validation – Any and all new methods developed must be procedurally recorded and validated.
- Specimen identification and collection – Every specimen must be recorded, including a description of how it was collected and stored.
- Histopathology – All records of any observed histopathological findings, must be meticulously kept.
- Data – All records related to the integrity, handling, storage and retrieval of data.
- Equipment, including software – records of maintenance, calibration and validation of all equipment and software.
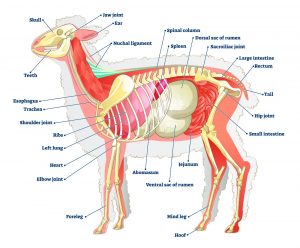
- All records involving animals, including any room preparation for animal care, as well as the transfer, placement and identification of the animals involved in the study.
As you can see, GLP is not a small endeavor and its importance in the progress and process of your product’s pre-clinical evaluation, is paramount. If you are aiming to have your product approved by the FDA or CE, it is essential to ensure that your study hermetically complies with GLP. LAHAV C.R.O. has the experience, knowledge and facilities, that guarantee that this very important step is done right and secured for your product’s advance.
- CFR – Code of Federal Regulations Title 21
- MBM Market Business News
- UF/Research
- LabManager